Four Pennsylvania-based health providers formalized clinical training affiliation agreements for students at Indiana University of Pennsylvania’s proposed college of osteopathic medicine.
The signings took place on November 21 at the IUP-Indiana Regional Medical Center’s third annual Pennsylvania Mountains Rural Health Conference, celebrating National Rural Health Day, held at IUP’s Kovalchick Convention and Athletic Complex and attended by more than 310 persons.

From left, George Garrow, CEO, Primary Health Network; Larry Nulton, CEO, Nulton Diagnostic and Treatment Center; Brian Stratta, CEO, Hyndman Area Health Center; John Roth, CEO, Broad Top Area Medical Center; IUP President Michael Driscoll; and Miko Rose, IUP founding dean of the proposed college of osteopathic medicine.
Valerie Arkoosh, secretary of Pennsylvania’s Department of Human Services, was the conference keynote speaker.
IUP’s Council of Trustees endorsed the exploration of a possible development of a college of osteopathic medicine at IUP in December 2022. IUP has formally initiated steps towards accreditation of its proposed college of osteopathic medicine from the American Osteopathic Association’s Commission on Osteopathic College Accreditation, a three- to five-year process that includes submission of self-studies and a feasibility study, along with site visits.
Securing clinical training sites for students is part of the successful accreditation process. Typically, students in colleges of osteopathic medicine spend the first two years of their education in the classroom; during the third and fourth years, students are based in the community at clinical sites.
Programs signing clinical training agreements on November 21 are Broad Top Area Medical Center, represented by CEO John Roth; Hyndman Area Health Centers, represented by CEO Brian Stratta; Nulton Diagnostics and Treatment Center, represented by CEO Larry Nulton; and Primary Health Network, represented by CEO George Garrow.
IUP signed its first clinical training affiliation agreement with Punxsutawney Area Hospital in June and its second clinical training affiliation agreement with IRMC in September.
“The proposed college of osteopathic medicine will be critical in addressing the need for rural health care providers in our commonwealth,” IUP President Michael Driscoll said. “The college’s founding leadership team are doing a great job of engaging partners in our shared vision. Today’s signing event continues to build on the already strong momentum for advancing the project.
“All four of these providers will offer unique and innovative training opportunities for our students, and we are grateful for their foresight and willingness to be part of the mission of preparing caring and experienced physicians for our communities, joining Punxsutawney Area Hospital and IRMC as clinical training sites,” he said. “IUP is grateful for the support, and we look forward to our students being part of the Broad Top, Hyndman, Nulton, and Primary Health Network programs.”

Valerie Arkoosh, secretary of Pennsylvania’s Department of Human Services, keynote speaker for IUP-Indiana Regional Medical Center’s third annual Pennsylvania Mountains Rural Health Conference.
“Broad Top Area Medical Center is excited to partner with Indiana University of Pennsylvania,” Roth said.
“As the healthcare industry continues to evolve, unfortunately, large areas of America, especially in rural communities like much of Pennsylvania, have become healthcare deserts, thus making it much more difficult to attract and retain primary care physicians to areas such as Huntingdon County where we are located. By providing necessary training in these medically underserved locations through the medical students’ field experience, we are hopeful that it may encourage them to consider practicing where there is great need. Broad Top is grateful that IUP is willing to step into this leadership role to train primary care physicians to practice in rural Pennsylvania communities.”
Broad Top Area Medical Center, a federally qualified health center, is a community-based and patient-directed organization that provides comprehensive primary health care and preventative care services. The physicians and providers specialize in medical and whole-person wellness programs. The Integrated Care Team offers expanded services for behavioral and mental health and podiatry and dental services. Broad Top Area Medical Center has locations at Broad Top, Cassville, Orbisonia, Huntingdon, Mount Union, Belleville, and Alexandria.
“As the CEO of Hyndman Area Health Centers, I am excited about the opportunity to partner with the IUP school of medicine,” Stratta said. “Together, we are committed to meeting the healthcare needs of our community by bringing much-needed physicians back to the rural areas we serve.”
Hyndman Area Health Center has offices in Hyndman, Bedford, Richland, Everett, and Johnstown. It offers a variety of health care, laboratory, and financial option resources in family medicine, pediatrics, dermatology, dental health, women’s health, behavioral health, chronic care management, and occupational health.
“We are thrilled to officially partner with Indiana University of Pennsylvania as a clinical partner,” Nulton said. “This collaboration represents a significant step in advancing mental health services and education in our community. At Nulton Diagnostic and Treatment Center, we are committed to fostering the next generation of mental health professionals while ensuring high-quality care for our patients. This partnership allows us to combine our expertise with IUP’s strong academic foundation, creating meaningful opportunities for students and impactful outcomes for those we serve.”
Aileen Oandasan, chief medical officer at Nulton Diagnostic and Treatment Center, also offered remarks during the signing ceremony.
Since 1995, the mental health specialists at Nulton Diagnostic and Treatment Center have provided effective, compassionate behavioral healthcare to children, adolescents, and adults. Its network of outpatient programs and services spans 16 counties and reaches more than 3,000 people every year. It offers services at 14 sites in Pennsylvania, including in Altoona, Bedford, Clarion, DuBois, Ebensburg, Greensburg, Johnstown, Milford, Philipsburg, Slatington, and Somerset.
“Primary Health Network is proud to partner with Indiana University of Pennsylvania to offer medical students invaluable hands-on experience within the Federally Qualified Health Center model of care,” Garrow said.
“This collaboration is a strategic effort to enhance the education and training of future physicians, particularly those who, like me, are from rural communities, ensuring they are well-prepared to deliver high-quality, patient-centered care in underserved communities. By bridging academic knowledge with real-world practice, this partnership is integral to the ongoing development of a skilled and compassionate healthcare workforce committed to meeting the diverse needs of the populations we serve.”
The Primary Health Network, a private, nonprofit organization, is Pennsylvania’s largest community health center and is one of the largest community health centers in the nation. PHN takes pride in providing quality healthcare services, regardless of circumstances. PHN began with one small community health center site in the Shenango Valley in 1984, with a central focus on providing the highest quality of care to the people served, and now includes nearly 50 health center sites located across Pennsylvania and northeast Ohio that offer patients access to a wide array of services, from primary to specialty care.
IRMC and Punxsutawney Area Hospital are members of the Pennsylvania Mountains Healthcare Alliance, a collaborative network of 17 independent community hospitals and healthcare centers.

Miko Rose, founding dean of IUP’s proposed college of osteopathic medicine
Miko Rose was hired as the founding dean of the proposed college of osteopathic medicine in November 2023; the hiring of a founding dean is one of the first steps to establishing the college. Rose, named one of Pennsylvania’s Fifty Over 50 by City & State Pennsylvania, is one of less than 150 physicians elected as a fellow of the American College of Neuropsychiatrists by the fellows of the American College of Neuropsychiatrists/American College of Osteopathic Neurologists and Psychiatrists.
“This was an incredibly impressive event today, with key community-based healthcare leaders joining Punxsutawney Area Hospital and IRMC as clinical training sites for our students,” Rose said. “These clinical training affiliation agreements show the broad community support and endorsement of our proposed college of osteopathic medicine, and these agreements continue to move us forward in our work, especially as we seek accreditation,” she said.
“All of our clinical training partners are fully committed to the values, mission, and approach for our proposed college of osteopathic medicine, including the importance of addressing mental health needs, which is all too often unavailable in rural areas,” she said.
“As we look to recruiting students who want to stay in underserved communities, it is important to have partners in place that share our commitment to federally underserved sites and a grassroots and compassionate approach to serving patients,” she said. “This allows us to emphasize outpatient primary care throughout our medical student training and helps us to create pipelines from rural communities to inspire students who would not have otherwise considered careers in medicine to follow this path. Those students will, in turn, be much more likely to serve in rural communities upon graduation,” Rose said.
In July, Ryan Smith joined the team as the founding associate dean of clinical affairs, responsible for overseeing the clinical curricular areas of the doctor of osteopathic medicine program, including developing clinical training agreements. In August, Luke H. Mortensen was hired as associate dean of preclinical affairs, responsible for overseeing the preclinical curricular areas of the program.
“We have been motivated and encouraged at the community-level support for this project,” Smith said.
“The clinical partnerships we have developed and that will mature have set us well on our way to ensuring resources to support the clinical education of our future medical students, with a strong emphasis on training sites located in truly rural settings, advancing our mission of improving access to quality healthcare for rural citizens of our state. We are well on track to meeting the necessary standards for accreditation,” he said.
IUP chose to explore a proposed college of osteopathic medicine based on several factors, including the critical need for rural health care: there are not enough trained physicians to provide care to Pennsylvania’s citizens: the ratio of patients to available primary care physicians is 1,367 to 1, according to the United Health Foundation.
There are only three colleges of osteopathic medicine in Pennsylvania, all at private universities; IUP’s proposed college of osteopathic medicine would be the only college of osteopathic medicine at a public university. National studies show that graduates from programs of osteopathic medicine are more likely to pursue primary care in rural and underserved areas—57 percent of all doctors of osteopathic medicine practice as general practitioners, and more than 20 percent of DO graduates practice in rural areas. Demand is high for osteopathic medicine training: in 2021, 22,708 applicants competed for 8,280 seats at schools of osteopathic medicine.
IUP’s proposed college of osteopathic medicine continues to draw support from individual donors, foundations, agencies, and legislators:
- In October, the Pennsylvania State System of Higher Education Board of Governors designated $2 million in design funds as part of the 2024–25 State System of Higher Education capital allocations budget for the academic building renovation for the health sciences cluster and proposed college of osteopathic medicine;
- Senator Joe Pittman and Representative Jim Struzzi announced in October that $2 million from the 2024–25 state budget has been set aside for the project;
- In July, IUP graduates Tim and Debra Phillips Cejka gifted $2 million;
- In June, the Foundation for IUP committed $20 million;
- In May, Congressman Guy Reschenthaler included $2 million for IUP’s project among his FY25 requested community projects, and Senator John Fetterman included $2 million on his list to advance in the FY25 Community Project Funding process;
- IUP received a $150,000 allocation for the project in the federal Consolidated Appropriations Act for Fiscal Year 2024, which was sponsored by Congressman Reschenthaler and Senator Fetterman and signed into law by President Joe Biden on March 9;
- In February, the Board of Governors allocated $500,000 for a facilities feasibility study for academic facilities for IUP’s health sciences cluster and proposed college of osteopathic medicine;
- In January, IUP’s Alumni Association Board of Directors authorized a donation of $500,000;
- In December 2023, Sen. Pittman announced that as part of the 2023–24 state budget, $2 million was set aside for the project;
- In July 2023, IUP graduates Nick Jacobs and Mary Ann Hoysan Jacobs donated $40,000 to advance the project. Nick Jacobs is a 2005 Distinguished Alumni Award recipient who has a 1969 bachelor’s degree in education and a 1972 master’s degree in music education; Mary Ann Jacobs has a 1968 bachelor’s degree in music education and a 1993 master’s degree in adult and community education; and
- In May 2023, Rich Caruso, a 1983 accounting graduate from Meadow Lands, 2023 Distinguished Alumni Award recipient and former president and current member of the Foundation for IUP Board of Directors and member of the Pennsylvania State System of Higher Education Board of Governors, announced a pledge of $1 million for the project.
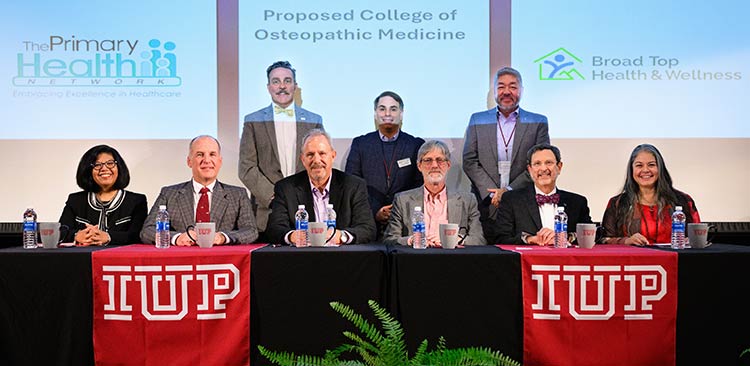
Seated from left: Aileen Oandasan, chief medical officer, Nulton Diagnostic and Treatment Center; Larry Nulton, CEO, Nulton Diagnostic and Treatment Center; Brian Stratta, CEO, Hyndman Area Health Center; John Roth, CEO, Broad Top Area Medical Center; IUP President Michael Driscoll; and Miko Rose, IUP founding dean of the proposed college of osteopathic medicine.
Standing from left: George Garrow, CEO, Primary Health Network; Ryan Smith, founding associate dean of clinical affairs of IUP’s proposed college of osteopathic medicine; and Luke H. Mortensen, founding associate dean of preclinical affairs, IUP proposed college of osteopathic medicine.
More About the Clinical Training Affiliation Sites
Broad Top Area Medical Center has full-service family practices dedicated to helping patients maintain and improve their health. The team of health professionals works together to serve the entire family for all health-related needs in all stages of life. The staff believes in providing comprehensive health care services to patients in a friendly, relaxed atmosphere and in educating patients to work together to achieve the best state of wellness possible.
Hyndman Area Health Center is the recipient of the HRSA Access Enhancer Award and the Health Disparities Reducer Award and is an FSHCAA Deemed Health Center. Its mission is to promote health and wellness to its patient population by providing patient-centered care that promotes engagement between the patient and the provider, leading to positive healthcare outcomes. HAHC, Inc., through its advocacy on behalf of the medically needy, provides a safety net for people facing financial, social, cultural, and language barriers in obtaining health care—medical, oral health, mental health, prescription assistance, and related medical services—by continuing to improve services and facilities and growing a financially sound and progressive community health center.
Each program at Nulton Diagnostic and Treatment Center is rooted in wellness, recovery, and open communication, creating a supportive healing environment that guides patients through every stage of treatment. The Center’s experienced team includes board-certified child and adult psychiatrists, licensed psychologists, therapists, licensed social workers, licensed professional counselors, registered nurses in psychiatry, licensed practical nurses, and other professionals specially trained to diagnose, treat, and manage behavioral health conditions. Its REACH Walk-in Center in Johnstown has a goal of making a positive difference in the lives of the individuals living with mental illness who reside in Cambria County through the coordination of supportive services for individuals and families seeking aid and intervention for individuals experiencing a mental health crisis or behavioral health emergency. Nulton Diagnostic and Treatment Center is accredited and certified by the Joint Commission on Accreditation of Healthcare Organizations and is a National Health Service CORPS facility.
After more than 40 years of service, the Primary Health Network has grown to become the largest Federally Qualified Health Center in Pennsylvania and one of the largest in the nation. Currently, PHN has a staff of more than 150 physicians, dentists, physician assistants, certified nurse practitioners, and other health professionals and a support staff of more than 450 employees. Since its beginnings, PHN has worked with local communities to develop and implement a new model of health care: the Community Health Center. Last year, PHN reached more than 75,000 patients through health, educational, and enabling services. It participates with the Age Friendly Health System.
At PHN, patients are the center of focus. PHN staff take various measures to ensure that patients receive the highest quality of care. Some initiatives include Primary Care Medical Home, free patient transportation to medical appointments in select counties (Beaver, Blair, Butler, Clarion, Erie, Jefferson, Lawrence, Mercer, and Mifflin), and continuing accreditation by the Joint Commission on the Accreditation of Healthcare Organizations. Adapting to the changing healthcare market, PHN participates in most managed care plans, processes most insurances, and offers a sliding fee discount to eligible patients. PHN has received awards and recognition from the Health Resources and Services Administration.
The PHN Charitable Foundation was established in 2005 to support the mission and goals of Primary Health Network. The Foundation supports this mission by raising funds to build and sustain programs that increase access to healthcare services and improve the health and quality of life in the communities PHN serves.